Birth Control
We get it; the world of contraception can feel like a maze, and you're just trying to find the right path. No worries, we've got your back. Choosing the right birth control method is a bit like finding the perfect playlist for a road trip: it should match your vibe, lifestyle, and, most importantly, keep you cruising smoothly.
Finding your contraceptive sidekick: types of birth control
There are a variety of birth control options available to suit different needs. These include hormonal methods like pills, patches, and implants, barrier methods such as condoms, and long-term options like IUDs. There are also permanent methods like sterilization and emergency contraception for backup. Natural methods involve tracking your cycle, while fertility awareness-based methods use signs to determine fertile days. The withdrawal method is another choice. To find the best fit for you, it's a good idea to have a friendly chat with a healthcare provider who can offer guidance based on your preferences and health considerations.



-
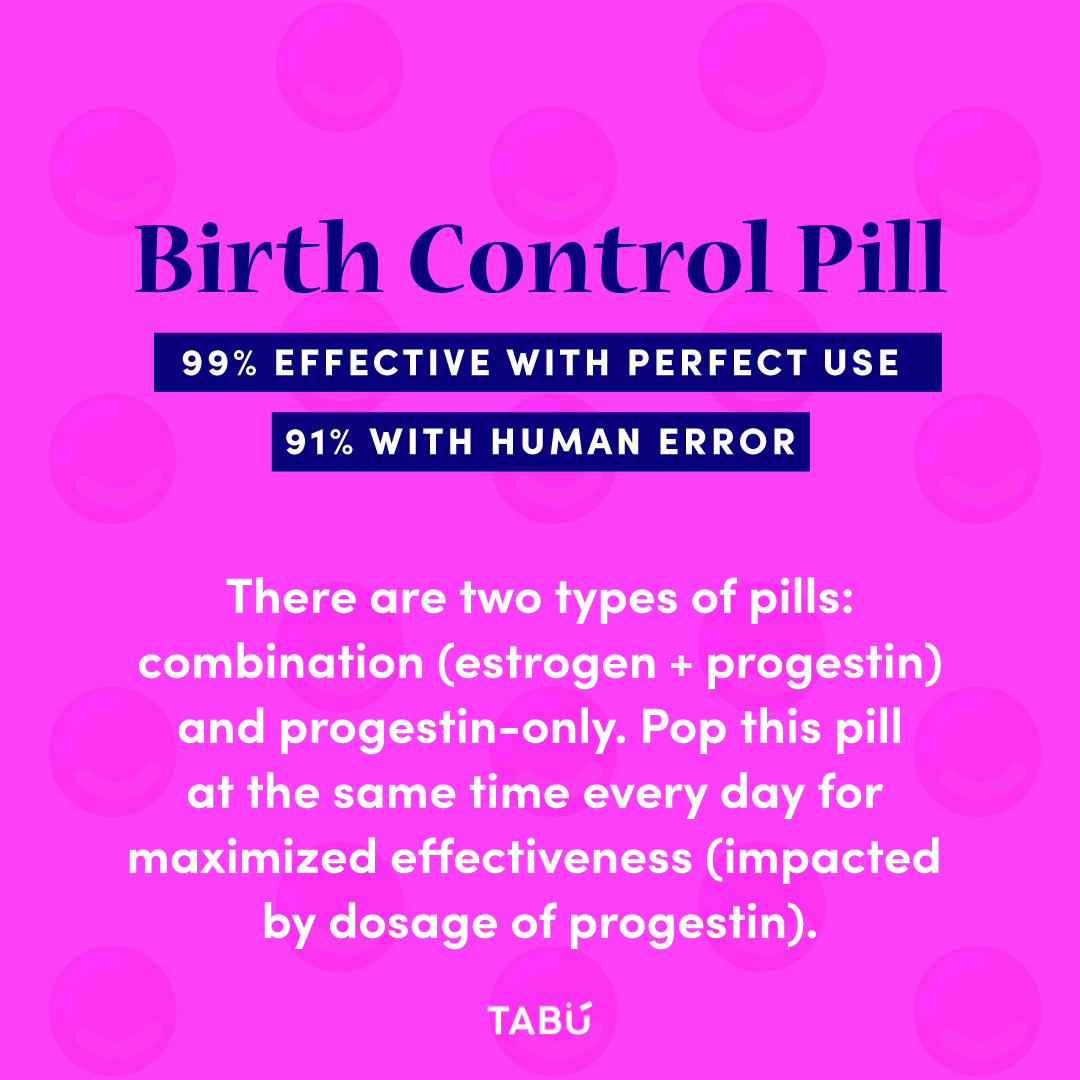
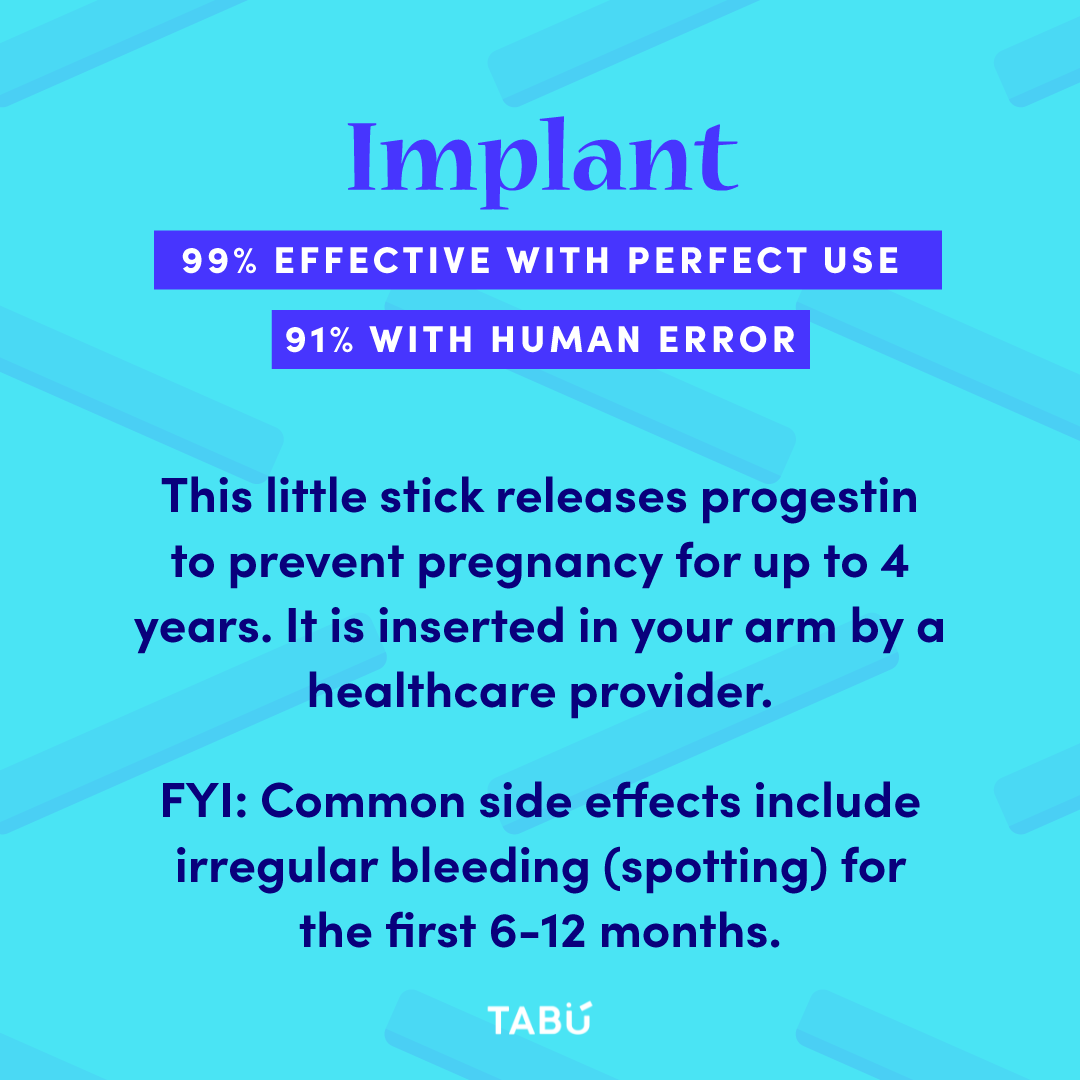
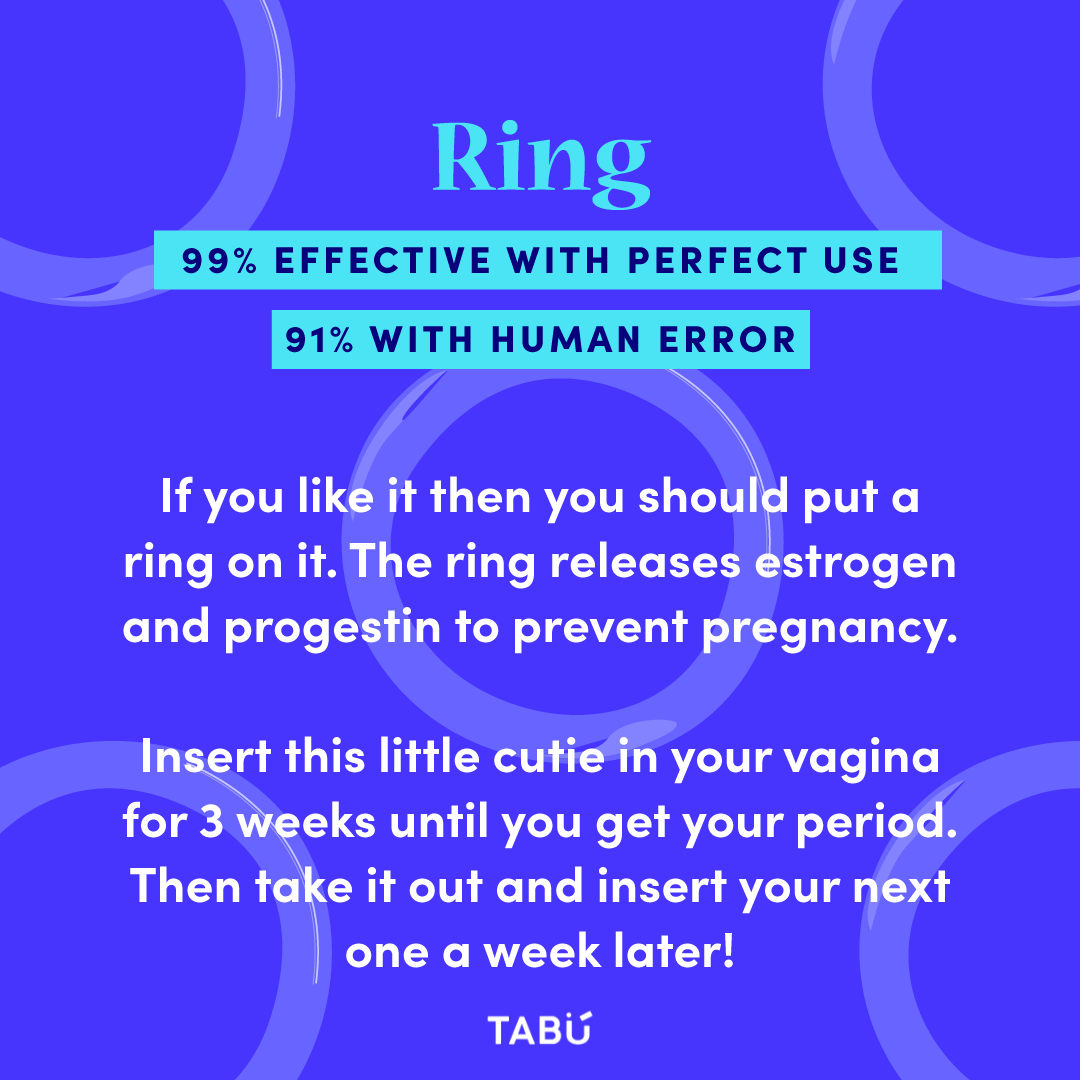
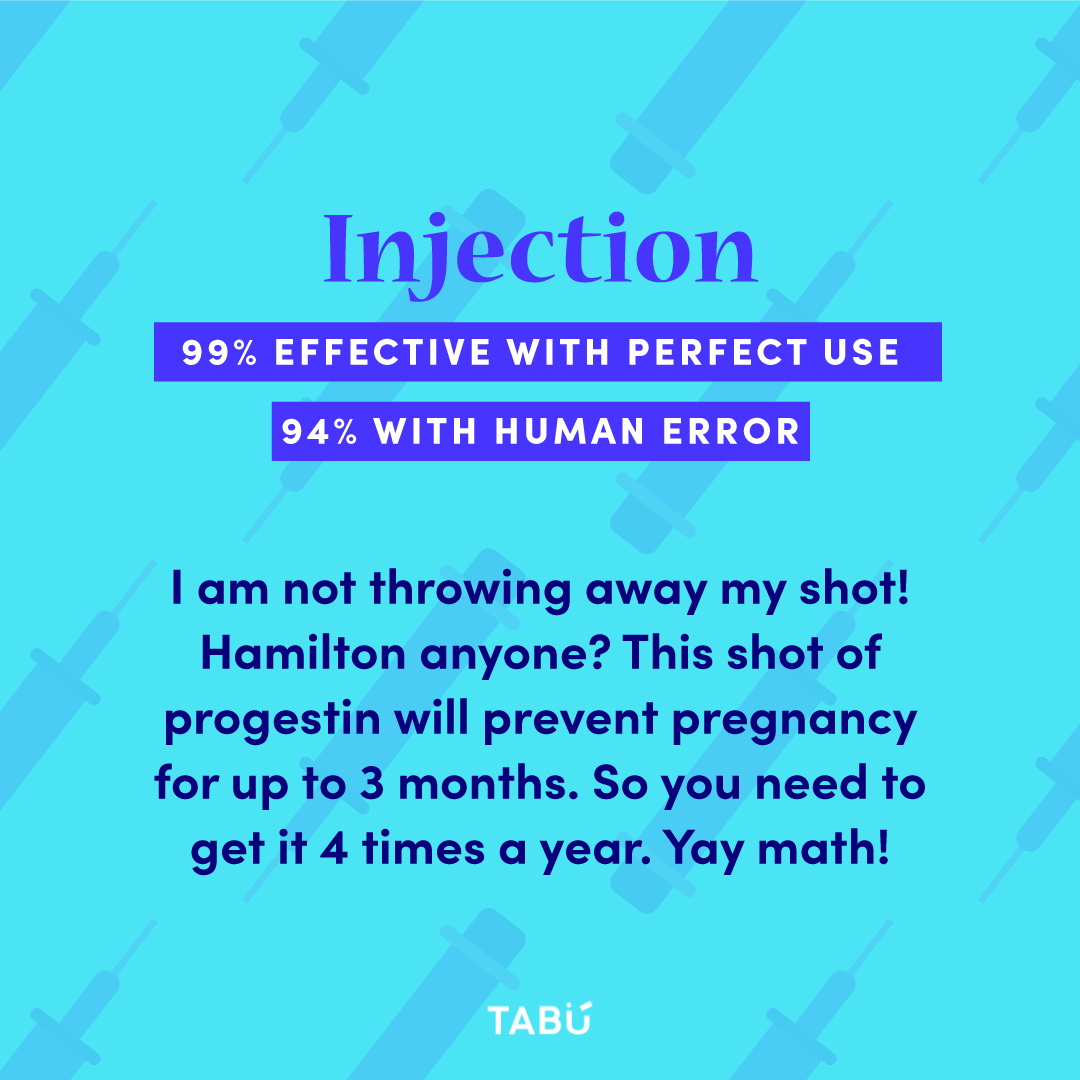
Today, there are numerous hormonal methods, including the Pill, Nexplanon, NuvaRing, the Patch (Ortho Evra), Depo-Provera, and intrauterine devices (IUDs). They work by preventing an egg from being released every month and thickening cervical mucus and thinning the lining of the uterus, thus inhibiting pregnancy by preventing sperm from entering your uterus. However, hormonal methods don’t protect against STIs. Also, if you’re taking the mini pill aka progestin-only pills (POP), it’s important to take the pill every day at the same time to maximize and ensure effectiveness!
-
If you like the benefits of the IUD, but are not comfortable with hormones, the non-hormonal (Copper) IUD might be the right option for you. The copper filament wrapped around the T prevents pregnancy by interfering with the sperm’s ability to reach the egg. Bear in mind, most people who use the Copper IUD tend to have heavier periods, especially for the first few months. You can also consider barrier methods, such as condoms, a non-hormonal birth control alternative.
-
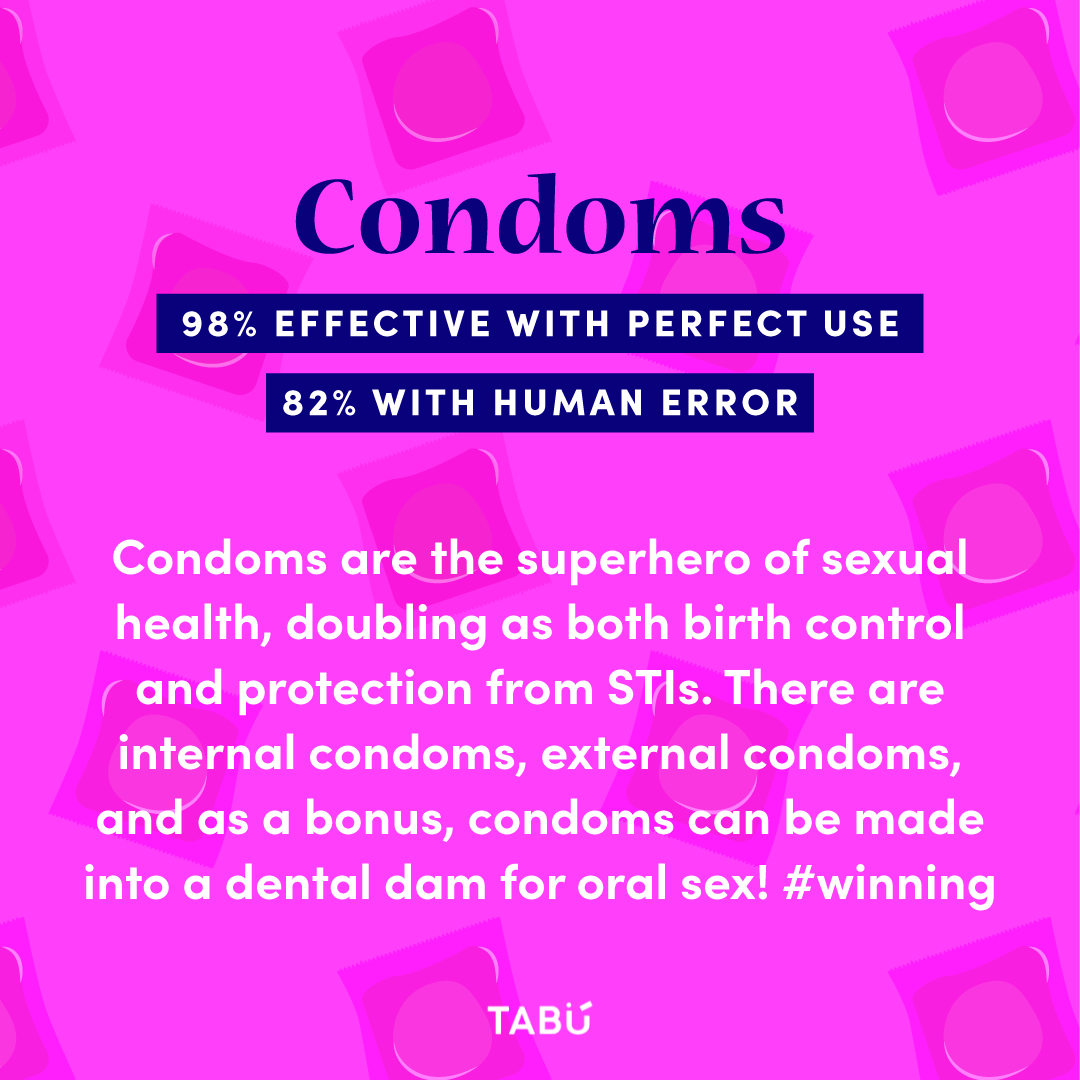
“Barrier method” options include a cervical cap, diaphragm, sponge, and internal or external condom. Out of all the types of contraceptives, the external condom is the most commonly used, as it offers protection against both STIs and unwanted pregnancy. Internal condoms, also known as “female” condoms, offer protection against STIs as well. For safety reasons, make sure you use a new condom each time you have sex — and be sure to check the expiration date!
-
“Don’t worry; I’ll just pull out.” OR NAH. The withdrawal/pull out/coitus interruptus method (so fancyl) is when a partner withdraws their penis from the vagina prior to ejaculation. Fun fact: about 35 million couples around the world rely on the withdrawal method. Wow! So, is it effective? If always done correctly, of every 100 women whose partners use withdrawal, 4 will become pregnant each year. Conversely, if not always done correctly (we are human after all), of every 100 women whose partners use withdrawal, 27 will become pregnant each year. While a convenient option, the withdrawal method requires a lot of experience, self-control, and trust. The partner with a penis must really know their sexual cycle (when they're going to ejaculate), and be able to exhibit maximized control. The withdrawal method is not recommended for individuals who experience premature ejaculation. It is also important to note that pregnancy can still occur if semen or pre-ejaculate/pre-cum is spilled on the vulva. The science on whether pre-cum can cause pregnancy is inconclusive, but studies suggest that it might, so it is at least worth acknowledging. Did we mention this method also doesn’t protect against STIs? (condoms for the win).
-
Although not a pill or device, the fertility awareness method (FAM) is still a contraceptive method. FAM is based on knowing the menstruating partner’s menstrual cycle so couples can avoid having sex (or use condoms) during periods of fertility. There are different ways to determine one’s most fertile time, including tracking your cycle, basal body temperature, and cervical mucus — keep in mind that higher protection rates occur when all three methods are used in combination. The effectiveness of this type of contraception varies because most people with a period don’t have a perfectly regular menstrual cycle. FAM also does not protect against STIs (sensing a theme here?).
-
The fertility awareness method (FAM) and natural family planning (NFP) are both methods of birth control that involve tracking your fertility signs to identify when you are most likely to get pregnant. However, there are some key differences between the two methods.
Fertility awareness method
FAM is a more general term that encompasses a variety of different methods for tracking fertility signs. Some of the most common FAM methods include:
Basal body temperature (BBT) method
Cervical mucus (CM) method
Symptothermal method
Ovulation predictor kits (OPKs)
FAM can be used to prevent pregnancy or to achieve pregnancy.
FAM users may choose to abstain from sex during their fertile days, or use a barrier method of birth control, such as condoms.
Natural family planning
NFP is a specific type of FAM often associated with methods that are approved by religious organizations.
NFP is based on the belief that sexual intercourse should only take place within the context of marriage and that it should be open to procreation.
NFP users tend to abstain from sex during their fertile days.
One of the key differences between FAM and NFP is that FAM can be used to prevent pregnancy or to achieve pregnancy, while NFP is only used to prevent pregnancy. Additionally, NFP users are generally expected to abstain from sex during their fertile days, while FAM users may choose to use a barrier method of birth control instead.
-
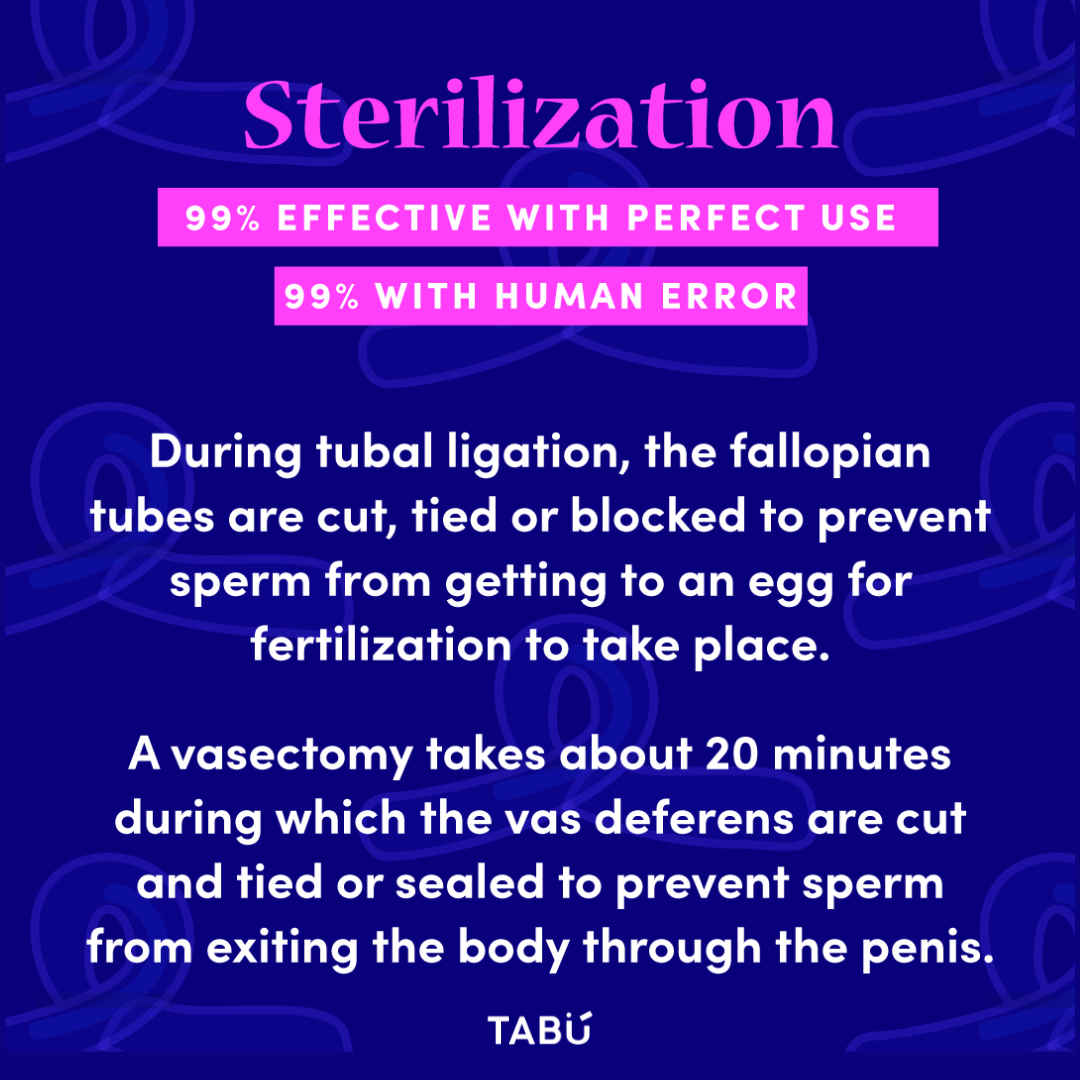
Sterilization methods prevent pregnancy by blocking reproductive functioning. They’re grouped into two categories: tubal ligation and vasectomy. Tubal ligation is a surgical procedure in which the fallopian tubes are clamped or severed, preventing eggs from reaching the uterus for implantation. A vasectomy consists of tying off and cutting the tubes that transport sperm. Both procedures are permanent and offer more than 99% protection against pregnancy (but none against STIs...just sayin' - don't forget condoms!). It’s worth noting that most vasectomies are reversible (though a reversal does not guarantee pregnancy viability).
-
Soooooo you’ve already had sex without birth control, or perhaps the condom broke. First of all, relax! Now is not the time to panic. If you are still within a 120 hour (5 day) window, you can take emergency contraception, colloquially known as the “morning-after pill,” to prevent pregnancy. Plan B is One-Step is the most well-known form of emergency contraception; you can get it at most drugstores or online. It is 95% effective within the first 24 hours, or about an 88% effective rate, on average, within 72 hours. Ella, also a pill, is 93-95% effective within 5 days. Ella requires a prescription from a doctor because it contains something called ulipristal acetate, which suppresses your body from producing progesterone, thereby delaying ovulation for up to 5 days (allowing sperm enough time to die before an egg is released). You can also get the copper (or non-hormonal) IUD inserted, which lowers your chances of getting pregnant by more than 99.9% if done within 5 days of unprotected sex. The copper IUD is the most effective form of emergency contraception, and can be left in for up to 12 years to help prevent future unwanted pregnancies. It is free under most insurance plans and Medicaid. Please read this Planned Parenthood article for more information on emergency contraception. If you have had unprotected sex, it is also wise to get tested for STIs, but not right away (different STIs can be detected in tests after different time periods after exposure to an infected partner). P.S. Emergency contraception is not the same thing as abortion, as it works before pregnancy begins. This is a common misconception to be aware of.
Illustration of birth control pills, by Marcy Gooberman
FAQ about birth control
-
First off, it's important to remember that everyone's body is unique, so the side effects can vary from person to person. But here are some common things you might experience when using hormonal birth control:
Change in Mood: Some folks notice mood swings, feeling a little up and down. It's like riding an emotional rollercoaster, but it usually levels out after a few months.
Nausea: Sometimes, especially when you start, birth control pills can make you feel a bit queasy. Taking them with food might help.
Breast Tenderness: Your boobs might feel a bit sore or swollen. It's like your body is adjusting, and this tends to go away after a while.
Changes in Periods: This one can be a game-changer for some. Your periods might become lighter, shorter, or even disappear altogether. But remember, not everyone experiences this, and it might take a few cycles to see these changes.
Headaches: Some people get headaches, but they often improve as your body adjusts.
Weight Fluctuations: A common myth is that birth control causes significant weight gain, but most studies suggest it's minimal, if any. Any weight changes are usually due to other factors.
Other Stuff: You might notice changes in your skin (sometimes for the better, thanks to fewer breakouts), or you might have some spotting between periods.
Remember, these side effects can be temporary, and your body often needs a little time to adapt. If you're concerned about any side effects, don't hesitate to reach out to your healthcare provider. They can help you find the right method that works for you or suggest some tweaks to minimize these effects.
Ultimately, it's all about what makes you feel comfortable and in control of your reproductive health. And remember, you're not alone in dealing with these questions – we've all been there at some point! 😊
-
STIs don’t feel too great either (even if there are no symptoms, no one wants an infection!). The greatest pleasure comes from peace of mind. If your partner is reluctant to use condoms, have a conversation, and be clear about your concerns. It’s your sex life, meaning you get to choose when, where, and how you want to have sex. If you are the partner that prefers not to wear condoms due to a feeling of decreased pleasure or comfort, consider trying out different kinds of condoms for fit and feel. Yes, condoms come in a variety of sizes; if it feels too tight or loose, you might just need a different size! You can also add a drop of lube in the tip of the condom before rolling it on to increase sensation (but not oil-based lube, as it degrades latex). If you are using a dental dam, apply lube directly on the vulva. Last tip: practicing masturbation with a condom on can help you get used to the feeling!
-
If you are 35 or older and smoke cigarettes or vape, it is not advised to use hormonal contraceptive methods such as the combination pill, the ring, or the patch. Vapes and cigarettes contain the same active ingredient (nicotine), which is known to elevate your blood pressure and heart rate and increase your risk of stroke or heart attack. If you smoke and you are under 35, let your health care provider know so they can help you make an informed decision about the best (non-hormonal) birth control option for you. Of course, we advise you to save your money (and your lungs), and quit smoking altogether! ❤
-
Abstinence, the practice of voluntarily refraining from sexual activity, is the only way to enjoy 100% protection from both STIs and pregnancy. Abstinence, by the way, is a completely fair choice (whether you have been sexually active before or not)! Remember, there are other ways to enjoy physical pleasure, including masturbation (with or without a partner), kissing, massages, etc.! Never let anyone pressure you into something you don’t want to do.
Knowledge, confidence, and communication are the key ingredients to delicious, safe, and satisfying sex. If you’re going to engage in sexual activity, take control of your sexual health and future by using contraception to prevent unintended pregnancies and STIs. With the peace of mind, you will enjoy sex a whole lot more!
tabú tip ❥
tabú tip ❥
Finding the right birth control option for you can take time. What works for your friend might not work the same for you; that’s okay! Discuss your options with your healthcare provider, and take our quiz to help you think about what might work best for you. Our handy summary cards can give you an overview to guide your conversation with your doctor as well. And don’t forget, condoms/dental dams are the best (and only, besides abstinence) method to protect against STIs!


Can a perfect fit condom can improve your sex life? (Yes, yes it can.)